I am a Chancellor's Fellow at the University of Edinburgh's Usher Institute, in the Centre for Medical Informatics.
My primary research interests include:
- Data Extraction from Electronic Health Records
- Machine Learning Classification Models for Medical Prognostic Modelling
- Estimating Medication Adherence from Primary Care Prescription Records
- Clinical Decision Support Tool Co-Design
- Understanding the Barriers and Facilitators of Clinical Decision Support Tool Adoption
Highlighted Publications
February, 2025

Five ways to enhance the diversity and quality of health data
Quattroni P, Routen A, Alderman J, Argent C, Cushworth S, Dambha-Miller H, Drummond R, Denniston A, Ganguli P,
Hamilton N, Ideh U, Khalid S, Kwok A, Laws E, Liu X, Nafilyan V, Palmer J, Pineda-Moncusi M, Sampri A, Tibble H, Torabi F,
Valabhji J, Withrow D, Welsh C, Wood AM, Akbari A & Khunti K
The UK Health Data Research Alliance presents five recommendations for improving data collection for inclusive health research.
The COVID-19 pandemic brought into sharp focus the effects of longstanding health inequalities and disproportionate disease burden
among some minority ethnic communities1. Ready availability of high-quality ethnicity data was key to enabling the detection of
differences in morbidity and mortality rates between different ethnic communities. Without accurate and comprehensive data, variations
in patients’ outcomes and in operational and clinical practices that affect ethnic groups cannot be identified, which means downstream
harms may go unrecognized. High-quality data on patients’ individual attributes, including ethnicity, are crucial to facilitating health
improvements for a multi-ethnic population.
 January, 2025
January, 2025

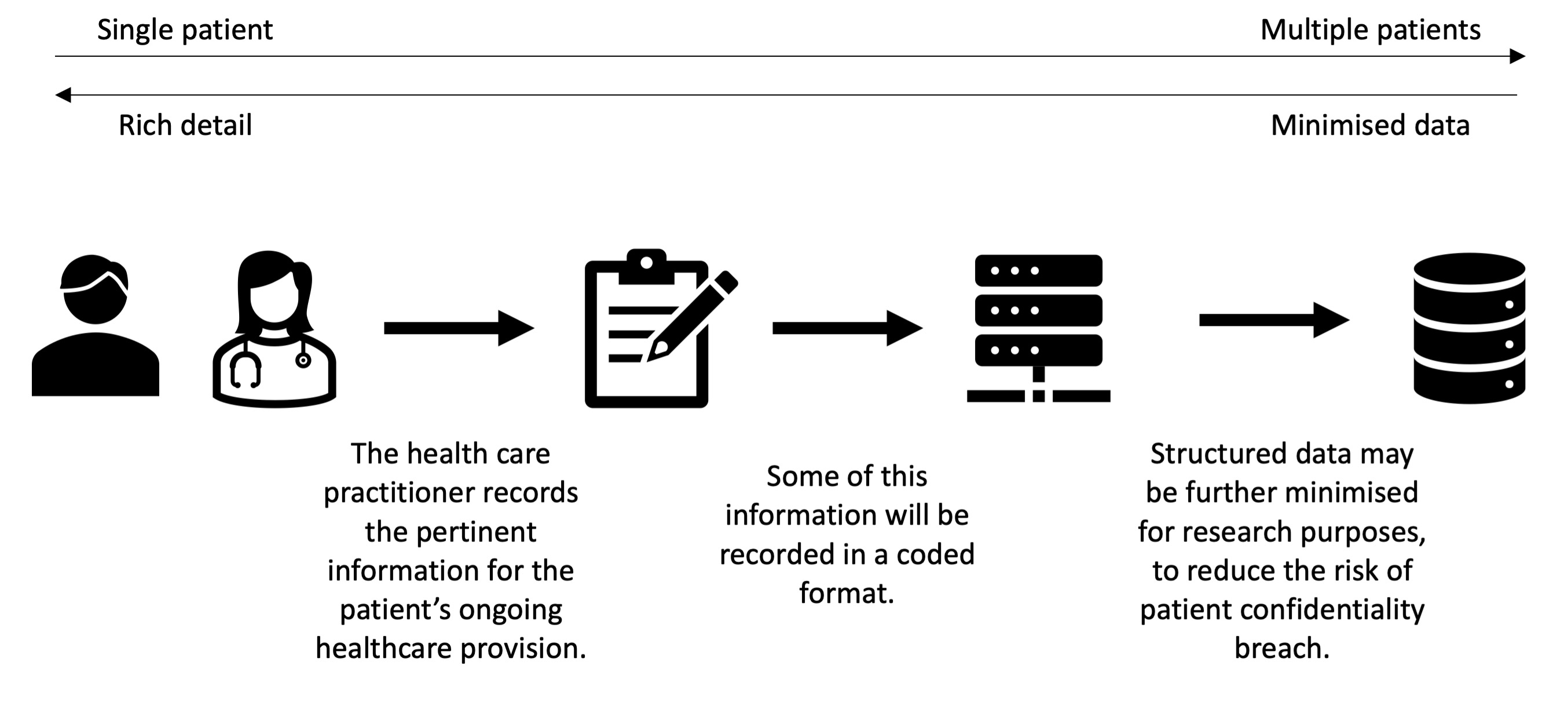
Using routine primary care data in research: (in)efficient case studies and perspectives from the Asthma UK Centre for Applied Research
Tibble H, Alyami R, Bush A, Cunningham S, Julious S, Price D, Quint JK, Turner S, Wang K, Wilson A, Davies GA,
Mukherjee M, Chan AHY, Varghese D, Jackson T, Morgan N, Daines L & Pinnock H.
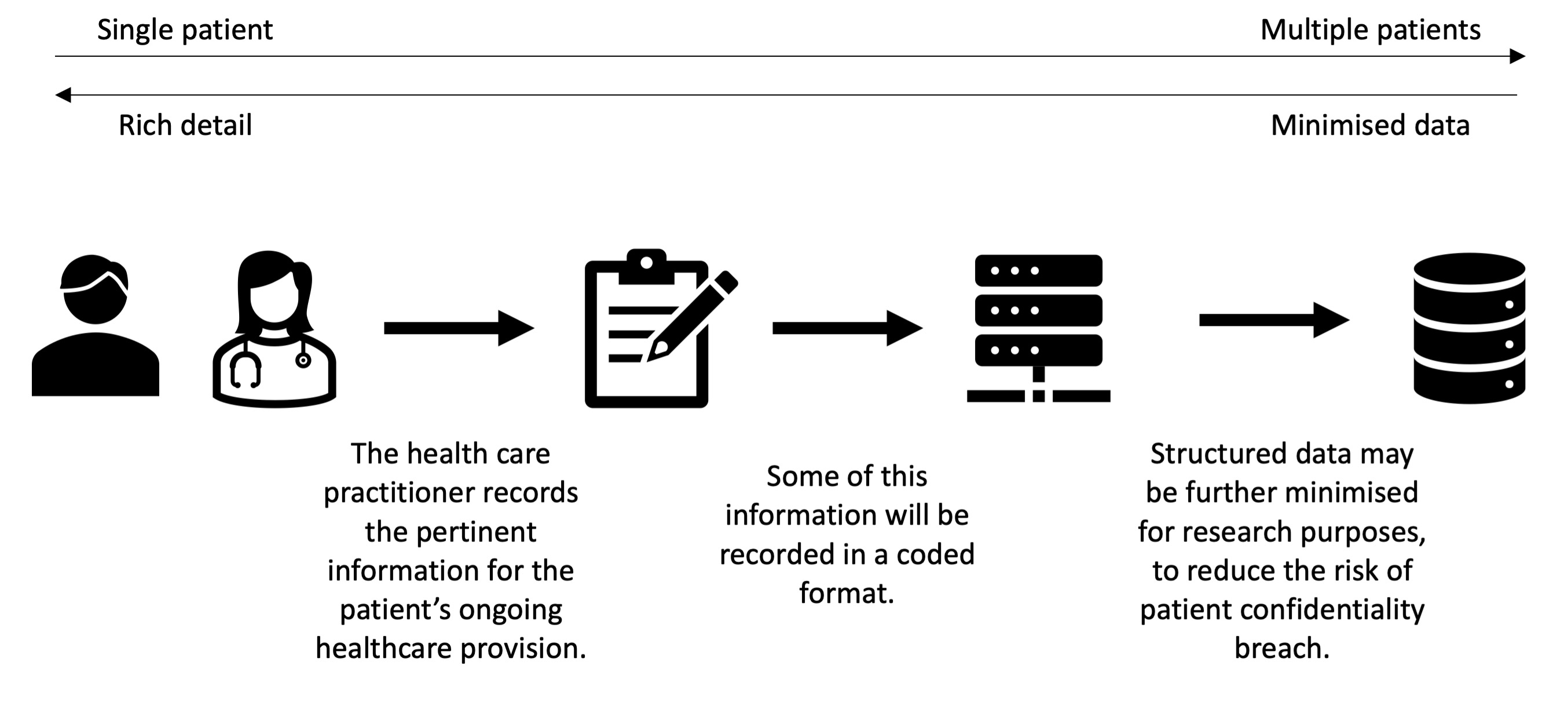
We aimed to identify enablers and barriers of using primary care routine data for healthcare research, to formulate recommendations for
improving efficiency in knowledge discovery. Data recorded routinely in primary care can be used for estimating the impact of interventions
provided within routine care for all people who are clinically eligible. Despite official promotion of ‘efficient trial designs’, anecdotally
researchers in the Asthma UK Centre for Applied Research (AUKCAR) have encountered multiple barriers to accessing and using routine data.
Using studies within the AUKCAR portfolio as exemplars, we captured limitations, barriers, successes, and strengths through correspondence
and discussions with the principal investigators and project managers of the case studies. We identified 14 studies (8 trials, 2 developmental
studies and 4 observational studies). Investigators agreed that using routine primary care data potentially offered a convenient collection
of data for effectiveness outcomes, health economic assessment and process evaluation in one data extraction. However, this advantage was
overshadowed by time-consuming processes that were major barriers to conducting efficient research. Common themes were multiple layers of
information governance approvals in addition to the ethics and local governance approvals required by all health service research; lack of
standardisation so that local approvals required diverse paperwork and reached conflicting conclusions as to whether a study should be approved.
Practical consequences included a trial that over-recruited by 20% in order to randomise 144 practices with all required permissions, and a
5-year delay in reporting a trial while retrospectively applied regulations were satisfied to allow data linkage. Overcoming the substantial
barriers of using routine primary care data will require a streamlined governance process, standardised understanding/application of regulations
and adequate National Health Service IT (Information Technology) capability. Without policy-driven prioritisation of these changes, the potential
of this valuable resource will not be leveraged.
 October, 2024
October, 2024

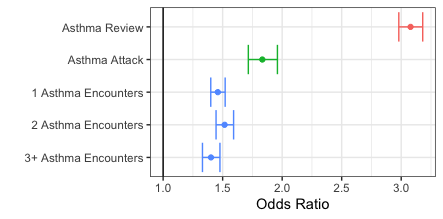
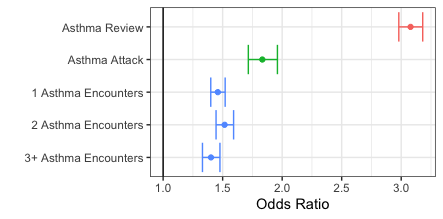
Prevalence and predictors of annual asthma reviews in Scottish primary care data
Tibble H & Chung A
People with asthma are recommended to have regular reviews in primary care, with assessment of symptoms, adjustment
of treatment and self-management processes, and the delivery of a written action plan for emergencies. Our study
aimed to investigate the incidence and factors associated with attendance of annual reviews. Electronic health
records for approximately 50 000 Scottish asthma patients, between 2008 and 2016. Multivariable logistic regression
using linked primary care prescription data and primary care registration demographic data. There was a median of
381 days between subsequent reviews. Reviews in the index year were strongly associated with reviews in the following
year (odds ratio 1.76 [1.68-1.84]). In contrast, asthma consultations (excluding reviews) in the index year were
associated with a lower odds of having a review in the following year (0.48 [0.46-0.51]). Those aged 18-35 in the
index year, or with missing address in the practice registration data, were the least likely age group to have an
asthma review in the following year. Reviewing the delivery of asthma care identifies patients who may be slipping
through the gaps by receiving only reactive asthma care rather than the structured, preventative care which can be
delivered through annual reviews. Understanding the risk factors for not receiving an annual review can be leveraged
to create more effective review invitations, such as explaining the specific content of reviews, introducing new
contact methods to improve health equity, and reviewing the algorithm used to determine who is invited.
 June, 2024
June, 2024

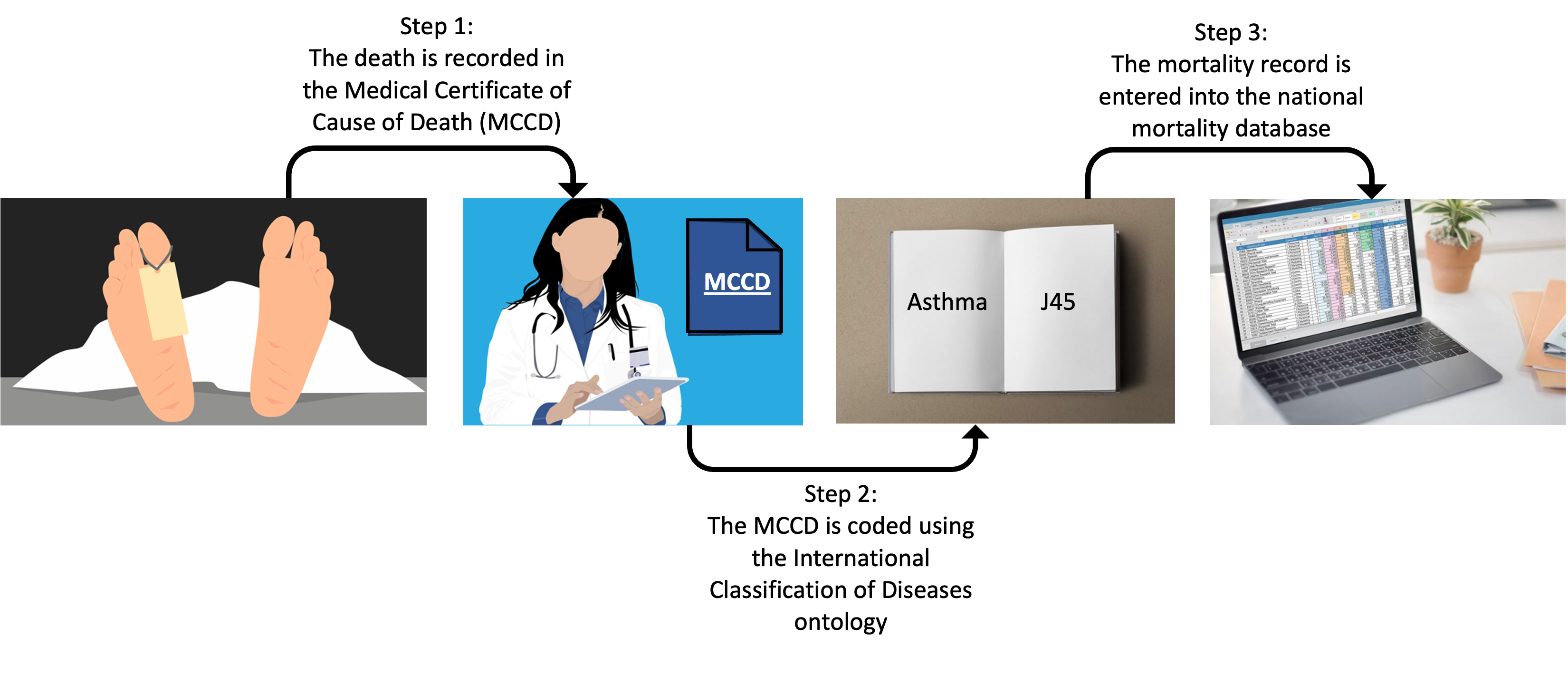
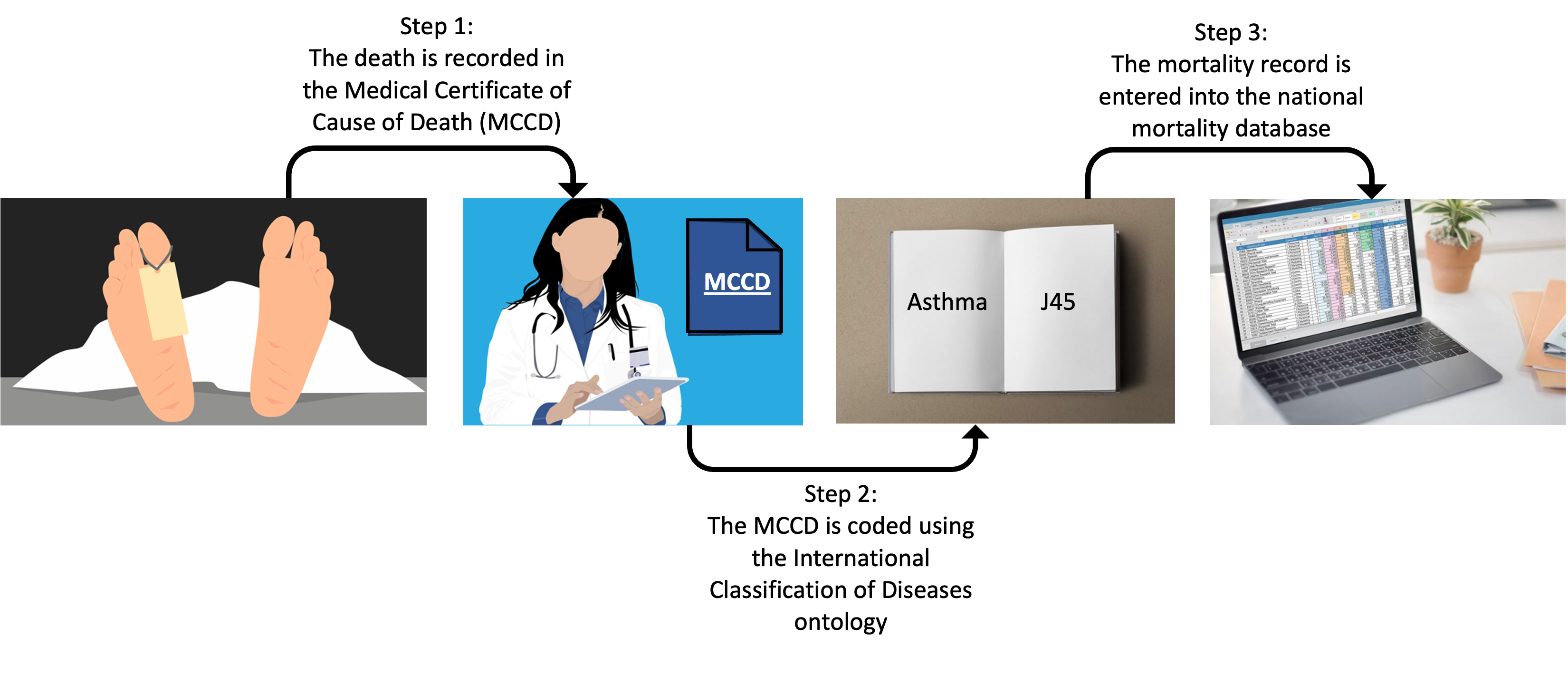
Cause of death coding in asthma
Chung A, Opoku-Pare GA & Tibble H
While clinical coding is intended to be an objective and standardized practice, it is important to recognize that it is not entirely the case.
The clinical and bureaucratic practices from event of death to a case being entered into a research dataset are important context for analysing
and interpreting this data. Variation in practices can influence the accuracy of the final coded record in two different stages: the reporting of
the death certificate, and the International Classification of Diseases (Version 10; ICD-10) coding of that certificate. This study investigated
91,022 deaths recorded in the Scottish Asthma Learning Healthcare System dataset between 2000 and 2017. Asthma-related deaths were identified by
the presence of any of ICD-10 codes J45 or J46, in any position. These codes were categorized either as relating to asthma attacks specifically
(status asthmatic; J46) or generally to asthma diagnosis (J45). We found that one in every 200 deaths in this were coded as being asthma related.
Less than 1% of asthma-related mortality records used both J45 and J46 ICD-10 codes as causes. Infection (predominantly pneumonia) was more
commonly reported as a contributing cause of death when J45 was the primary coded cause, compared to J46, which specifically denotes asthma attacks.
Further inspection of patient history can be essential to validate deaths recorded as caused by asthma, and to identify potentially mis-recorded
non-asthma deaths, particularly in those with complex comorbidities.
 June, 2024
June, 2024

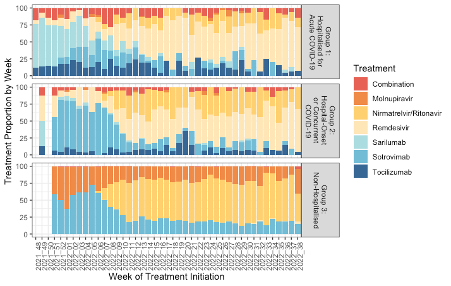
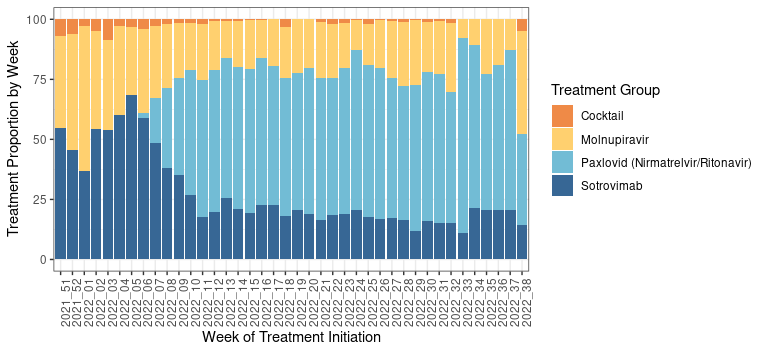
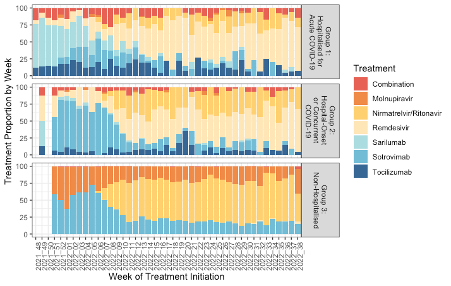
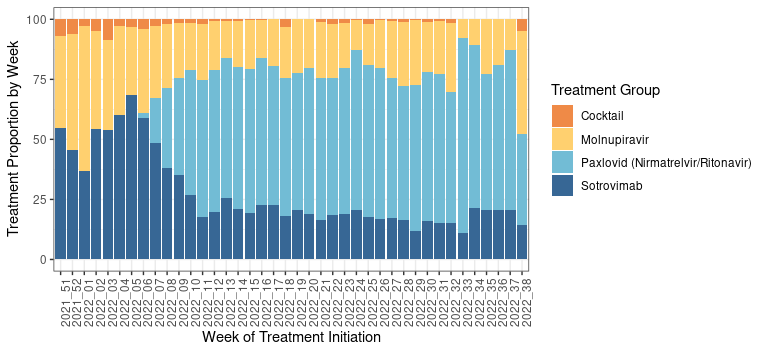
Real-world severe COVID-19 outcomes associated with use of antivirals and neutralising monoclonal antibodies in Scotland
Tibble H, Mueller T, Proud E, Hall E, Kurdi A, Robertson C, Bennie M, Woolford L, Laidlaw L, Sterniczuk K, Sheikh A
We sought to investigate the incidence of severe COVID-19 outcomes after treatment with antivirals and neutralising monoclonal antibodies, and estimate
the comparative effectiveness of treatments in community-based individuals. We conducted a retrospective cohort study investigating clinical outcomes
of hospitalisation, intensive care unit admission and death, in those treated with antivirals and monoclonal antibodies for COVID-19 in Scotland between
December 2021 and September 2022. We compared the effect of various treatments on the risk of severe COVID-19 outcomes, stratified by most prevalent
sub-lineage at that time, and controlling for comorbidities and other patient characteristics. We identified 14,365 individuals treated for COVID-19
during our study period, some of whom were treated for multiple infections. The incidence of severe COVID-19 outcomes (inpatient admission or death)
in community-treated patients (81% of all treatment episodes) was 1.2% (n = 137/11894, 95% CI 1.0-1.4), compared to 32.8% in those treated in hospital
for acute COVID-19 (re-admissions or death; n = 40/122, 95% CI 25.1-41.5). For community-treated patients, there was a lower risk of severe outcomes
(inpatient admission or death) in younger patients, and in those who had received three or more COVID-19 vaccinations.
 July, 2023
July, 2023

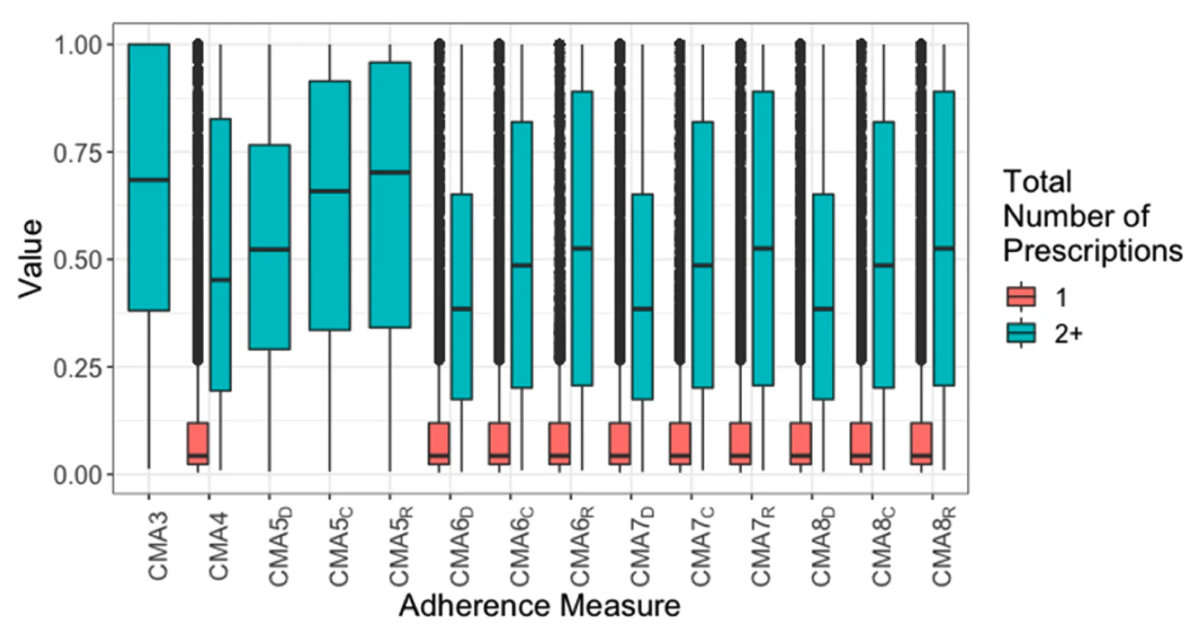
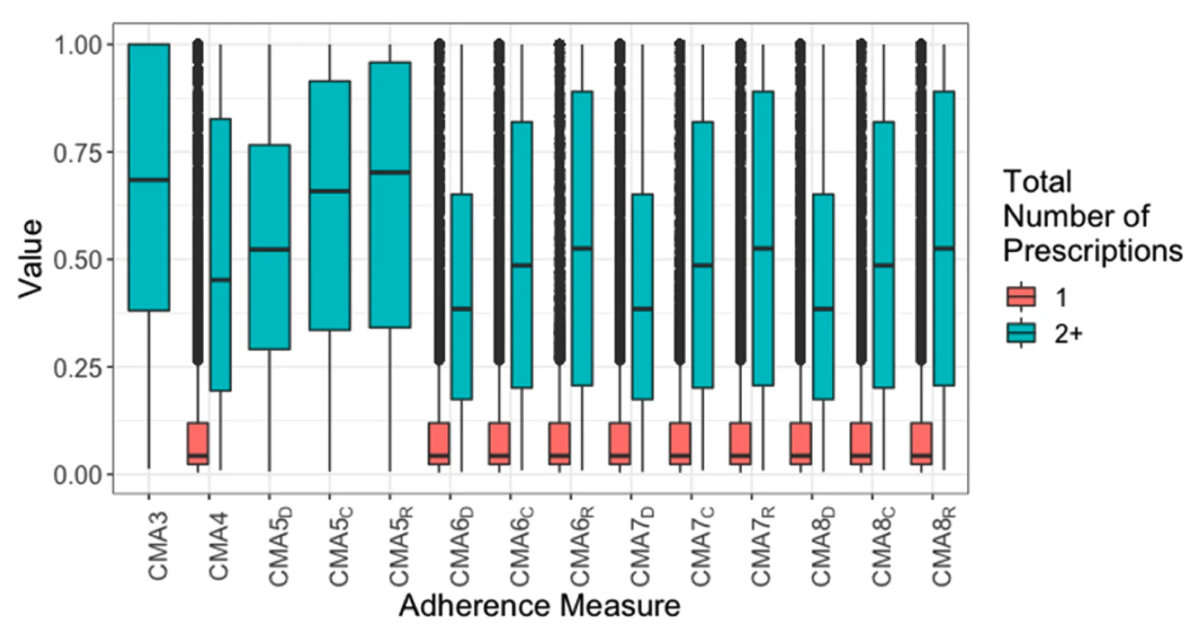
Estimating medication adherence from Electronic Health Records: comparing methods for mining and processing asthma treatment prescriptions
Tibble H, Sheikh A, Tsanas A.
We evaluated the limitations of various medication adherence measures, and highlight key considerations about the underlying data, condition, and population to
guide researchers choose appropriate adherence measures. This guidance will enable researchers to make more informed decisions about the methodology they employ,
ensuring that adherence is captured in the most meaningful way for their particular application needs.
 March, 2023
March, 2023

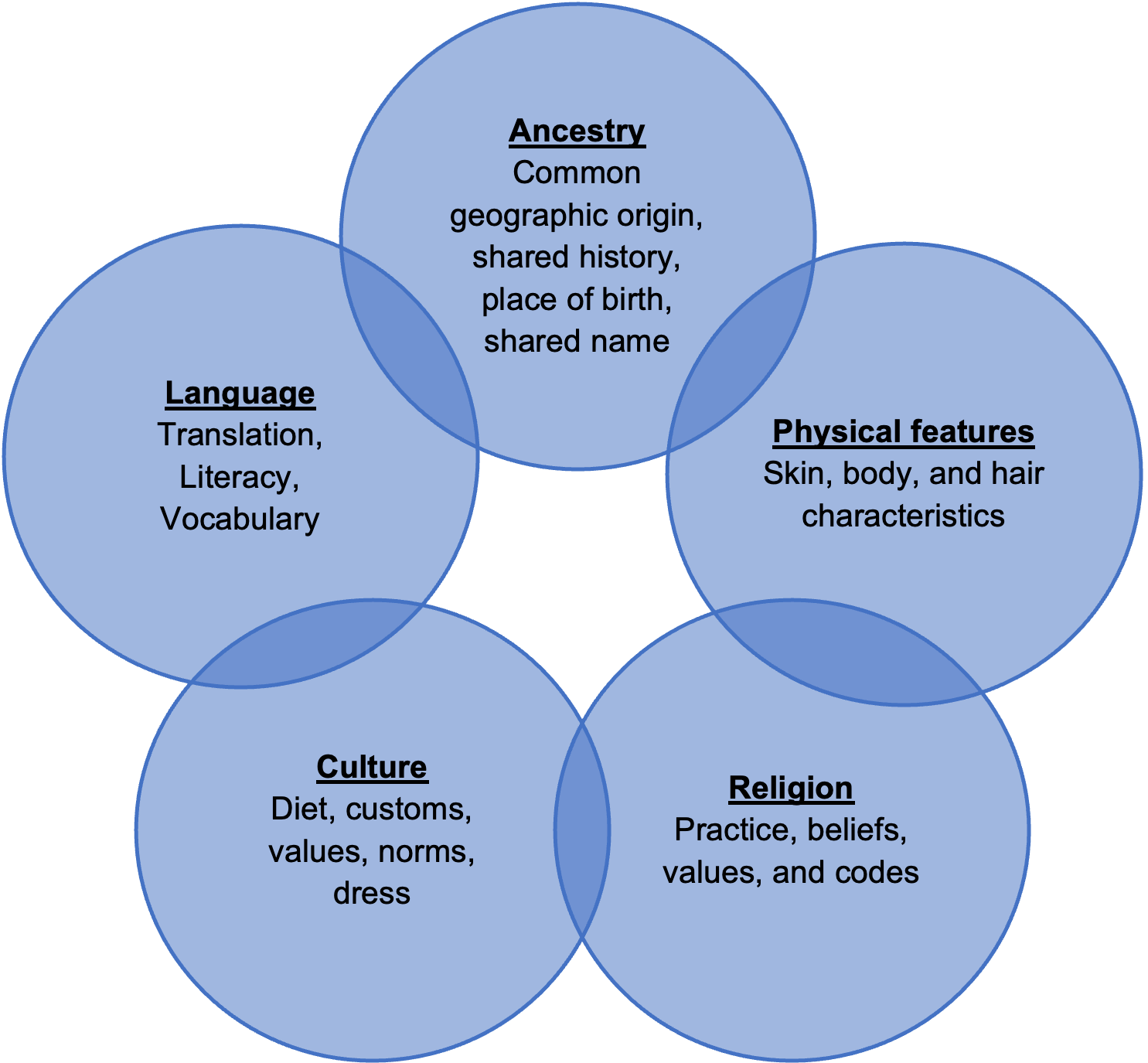
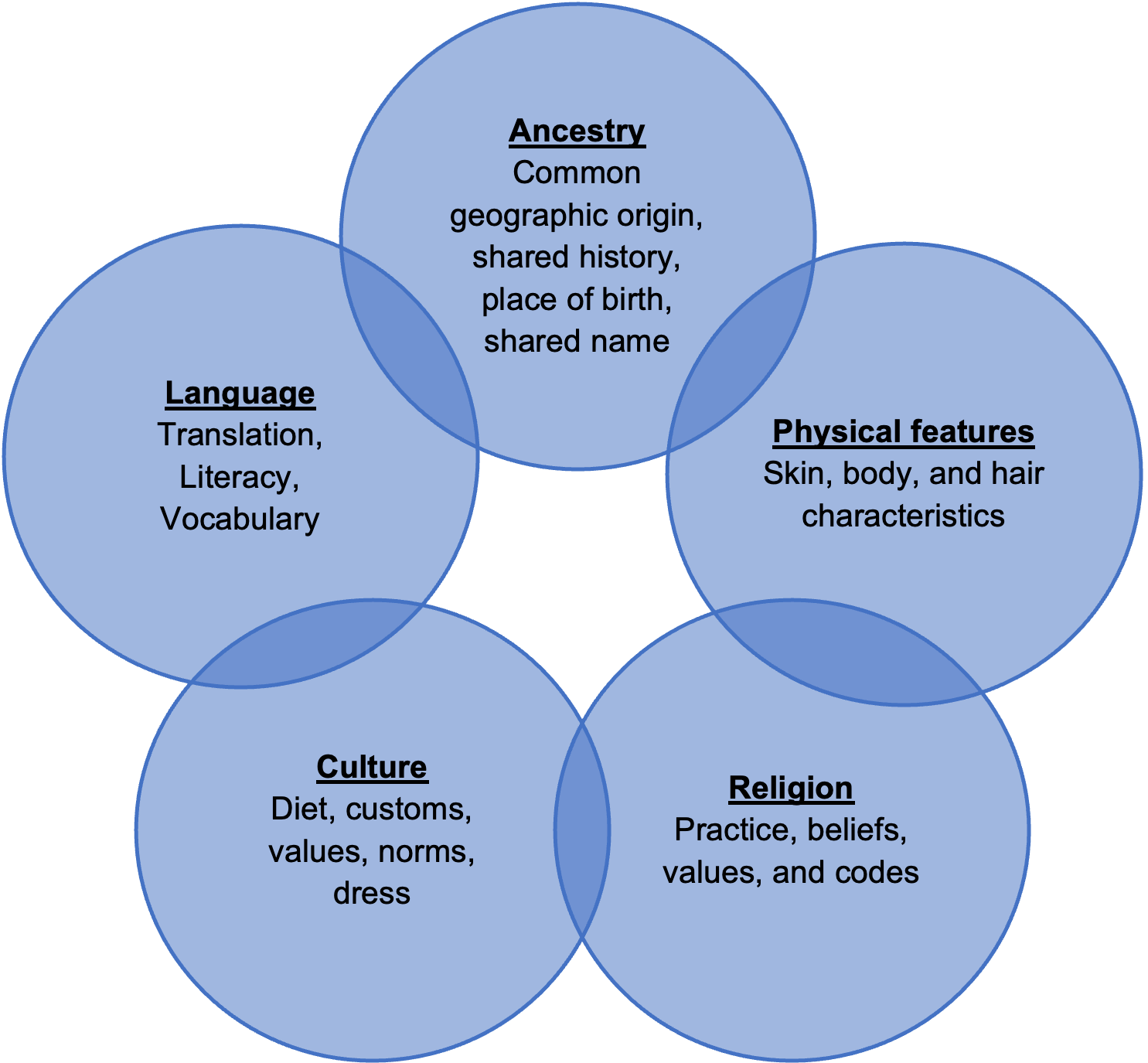
Ethnic, racial and migrant inequalities in respiratory health
Tibble H, Daines L, Sheikh A.
Disparities in the incidence, prevalence, morbidity and mortality rates of many respiratory diseases are evident between ethnic groups.
Biological, cultural, and environmental factors related to ethnicity can all contribute to the differences in respiratory health observed
between ethnic minority groups, but inequalities observed are most commonly due to lower socio-economic status. People who migrate within
a country or across an international border may experience an improvement in respiratory health associated with improvements in socioeconomic
status. However, migrants may also experience worse health outcomes in destination countries, as they are faced by barriers in language and
culture, discrimination, exclusion, and limited access to health services. Whilst some high quality studies investigating ethnicity and
respiratory health are available, further research into ethnic differences is needed. Improving the recording of ethnicity in health records,
addressing barriers to accessing respiratory health care and improving cultural literacy more generally are some of the ways that inequalities
can be tackled.
 December, 2022
December, 2022

Uptake of monoclonal antibodies and antiviral therapies for COVID-19 in Scotland
Tibble H, Mueller T, Proud E, Hall E, Kurdi A, Robertson C, Bennie M, Woolford L, Sheikh A.
There is a clear need to increase uptake of COVID-19 treatment options in individuals who are at high risk of severe COVID-19 outcomes —
particularly those who are younger than 18 years, are socioeconomically disadvantaged, have HIV and particular rheumatological conditions,
or have suboptimal protection from vaccination.

Five ways to enhance the diversity and quality of health data
Quattroni P, Routen A, Alderman J, Argent C, Cushworth S, Dambha-Miller H, Drummond R, Denniston A, Ganguli P, Hamilton N, Ideh U, Khalid S, Kwok A, Laws E, Liu X, Nafilyan V, Palmer J, Pineda-Moncusi M, Sampri A, Tibble H, Torabi F, Valabhji J, Withrow D, Welsh C, Wood AM, Akbari A & Khunti K
The UK Health Data Research Alliance presents five recommendations for improving data collection for inclusive health research. The COVID-19 pandemic brought into sharp focus the effects of longstanding health inequalities and disproportionate disease burden among some minority ethnic communities1. Ready availability of high-quality ethnicity data was key to enabling the detection of differences in morbidity and mortality rates between different ethnic communities. Without accurate and comprehensive data, variations in patients’ outcomes and in operational and clinical practices that affect ethnic groups cannot be identified, which means downstream harms may go unrecognized. High-quality data on patients’ individual attributes, including ethnicity, are crucial to facilitating health improvements for a multi-ethnic population.


Using routine primary care data in research: (in)efficient case studies and perspectives from the Asthma UK Centre for Applied Research
Tibble H, Alyami R, Bush A, Cunningham S, Julious S, Price D, Quint JK, Turner S, Wang K, Wilson A, Davies GA, Mukherjee M, Chan AHY, Varghese D, Jackson T, Morgan N, Daines L & Pinnock H.
We aimed to identify enablers and barriers of using primary care routine data for healthcare research, to formulate recommendations for improving efficiency in knowledge discovery. Data recorded routinely in primary care can be used for estimating the impact of interventions provided within routine care for all people who are clinically eligible. Despite official promotion of ‘efficient trial designs’, anecdotally researchers in the Asthma UK Centre for Applied Research (AUKCAR) have encountered multiple barriers to accessing and using routine data. Using studies within the AUKCAR portfolio as exemplars, we captured limitations, barriers, successes, and strengths through correspondence and discussions with the principal investigators and project managers of the case studies. We identified 14 studies (8 trials, 2 developmental studies and 4 observational studies). Investigators agreed that using routine primary care data potentially offered a convenient collection of data for effectiveness outcomes, health economic assessment and process evaluation in one data extraction. However, this advantage was overshadowed by time-consuming processes that were major barriers to conducting efficient research. Common themes were multiple layers of information governance approvals in addition to the ethics and local governance approvals required by all health service research; lack of standardisation so that local approvals required diverse paperwork and reached conflicting conclusions as to whether a study should be approved. Practical consequences included a trial that over-recruited by 20% in order to randomise 144 practices with all required permissions, and a 5-year delay in reporting a trial while retrospectively applied regulations were satisfied to allow data linkage. Overcoming the substantial barriers of using routine primary care data will require a streamlined governance process, standardised understanding/application of regulations and adequate National Health Service IT (Information Technology) capability. Without policy-driven prioritisation of these changes, the potential of this valuable resource will not be leveraged.

Prevalence and predictors of annual asthma reviews in Scottish primary care data
Tibble H & Chung A
People with asthma are recommended to have regular reviews in primary care, with assessment of symptoms, adjustment of treatment and self-management processes, and the delivery of a written action plan for emergencies. Our study aimed to investigate the incidence and factors associated with attendance of annual reviews. Electronic health records for approximately 50 000 Scottish asthma patients, between 2008 and 2016. Multivariable logistic regression using linked primary care prescription data and primary care registration demographic data. There was a median of 381 days between subsequent reviews. Reviews in the index year were strongly associated with reviews in the following year (odds ratio 1.76 [1.68-1.84]). In contrast, asthma consultations (excluding reviews) in the index year were associated with a lower odds of having a review in the following year (0.48 [0.46-0.51]). Those aged 18-35 in the index year, or with missing address in the practice registration data, were the least likely age group to have an asthma review in the following year. Reviewing the delivery of asthma care identifies patients who may be slipping through the gaps by receiving only reactive asthma care rather than the structured, preventative care which can be delivered through annual reviews. Understanding the risk factors for not receiving an annual review can be leveraged to create more effective review invitations, such as explaining the specific content of reviews, introducing new contact methods to improve health equity, and reviewing the algorithm used to determine who is invited.

Cause of death coding in asthma
Chung A, Opoku-Pare GA & Tibble H
While clinical coding is intended to be an objective and standardized practice, it is important to recognize that it is not entirely the case. The clinical and bureaucratic practices from event of death to a case being entered into a research dataset are important context for analysing and interpreting this data. Variation in practices can influence the accuracy of the final coded record in two different stages: the reporting of the death certificate, and the International Classification of Diseases (Version 10; ICD-10) coding of that certificate. This study investigated 91,022 deaths recorded in the Scottish Asthma Learning Healthcare System dataset between 2000 and 2017. Asthma-related deaths were identified by the presence of any of ICD-10 codes J45 or J46, in any position. These codes were categorized either as relating to asthma attacks specifically (status asthmatic; J46) or generally to asthma diagnosis (J45). We found that one in every 200 deaths in this were coded as being asthma related. Less than 1% of asthma-related mortality records used both J45 and J46 ICD-10 codes as causes. Infection (predominantly pneumonia) was more commonly reported as a contributing cause of death when J45 was the primary coded cause, compared to J46, which specifically denotes asthma attacks. Further inspection of patient history can be essential to validate deaths recorded as caused by asthma, and to identify potentially mis-recorded non-asthma deaths, particularly in those with complex comorbidities.

Real-world severe COVID-19 outcomes associated with use of antivirals and neutralising monoclonal antibodies in Scotland
Tibble H, Mueller T, Proud E, Hall E, Kurdi A, Robertson C, Bennie M, Woolford L, Laidlaw L, Sterniczuk K, Sheikh A
We sought to investigate the incidence of severe COVID-19 outcomes after treatment with antivirals and neutralising monoclonal antibodies, and estimate the comparative effectiveness of treatments in community-based individuals. We conducted a retrospective cohort study investigating clinical outcomes of hospitalisation, intensive care unit admission and death, in those treated with antivirals and monoclonal antibodies for COVID-19 in Scotland between December 2021 and September 2022. We compared the effect of various treatments on the risk of severe COVID-19 outcomes, stratified by most prevalent sub-lineage at that time, and controlling for comorbidities and other patient characteristics. We identified 14,365 individuals treated for COVID-19 during our study period, some of whom were treated for multiple infections. The incidence of severe COVID-19 outcomes (inpatient admission or death) in community-treated patients (81% of all treatment episodes) was 1.2% (n = 137/11894, 95% CI 1.0-1.4), compared to 32.8% in those treated in hospital for acute COVID-19 (re-admissions or death; n = 40/122, 95% CI 25.1-41.5). For community-treated patients, there was a lower risk of severe outcomes (inpatient admission or death) in younger patients, and in those who had received three or more COVID-19 vaccinations.

Estimating medication adherence from Electronic Health Records: comparing methods for mining and processing asthma treatment prescriptions
Tibble H, Sheikh A, Tsanas A.
We evaluated the limitations of various medication adherence measures, and highlight key considerations about the underlying data, condition, and population to guide researchers choose appropriate adherence measures. This guidance will enable researchers to make more informed decisions about the methodology they employ, ensuring that adherence is captured in the most meaningful way for their particular application needs.

Ethnic, racial and migrant inequalities in respiratory health
Tibble H, Daines L, Sheikh A.
Disparities in the incidence, prevalence, morbidity and mortality rates of many respiratory diseases are evident between ethnic groups. Biological, cultural, and environmental factors related to ethnicity can all contribute to the differences in respiratory health observed between ethnic minority groups, but inequalities observed are most commonly due to lower socio-economic status. People who migrate within a country or across an international border may experience an improvement in respiratory health associated with improvements in socioeconomic status. However, migrants may also experience worse health outcomes in destination countries, as they are faced by barriers in language and culture, discrimination, exclusion, and limited access to health services. Whilst some high quality studies investigating ethnicity and respiratory health are available, further research into ethnic differences is needed. Improving the recording of ethnicity in health records, addressing barriers to accessing respiratory health care and improving cultural literacy more generally are some of the ways that inequalities can be tackled.

Uptake of monoclonal antibodies and antiviral therapies for COVID-19 in Scotland
Tibble H, Mueller T, Proud E, Hall E, Kurdi A, Robertson C, Bennie M, Woolford L, Sheikh A.
There is a clear need to increase uptake of COVID-19 treatment options in individuals who are at high risk of severe COVID-19 outcomes — particularly those who are younger than 18 years, are socioeconomically disadvantaged, have HIV and particular rheumatological conditions, or have suboptimal protection from vaccination.
Thanks to Jack Turner for the website template.